Malignant gastrointestinal neuroectodermal tumor (GNET), formerly known as clear cell sarcoma of the gastrointestinal tract, is an extremely rare tumor of mesenchymal origin, which presents great microscopic and molecular similarity to clear cell sarcoma found in other parts of the body, such as tendons and aponeurosis. It is characterized by its rapid evolution, high recurrence rate and frequent diagnosis as metastatic disease.1,2
Keywords: malignant neuroectodermal tumor of the gastrointestinal tract, GNET, clear cell sarcoma, EWRS1, S-100 protein.
Malignant gastrointestinal neuroectodermal tumor (GNET), formerly known as clear cell sarcoma of the gastrointestinal tract, is an extremely rare tumor of mesenchymal origin, which presents great microscopic and molecular similarity to clear cell sarcoma found in other parts of the body, such as tendons and aponeurosis. It is characterized by its rapid evolution, high recurrence rate and frequent diagnosis as metastatic disease.1,2
A 22-year-old female patient with no relevant clinical history consulted for abdominal pain of 48 hours duration. On physical examination, a hard mass was palpable on the right flank, with diffuse rebound pain and guarding.
CT scan of the abdomen and pelvis showed a polylobulated mass with soft tissue density, measuring 80x60x90 mm, at the level of the mesentery in projection of the right mesocolon, and a small amount of fluid in the cul- de-sac of Douglas. The laboratory showed hematocrit 25%, hemoglobin 7.1 g/dl, leukocytosis and thrombocytosis.
Given the impossibility of ruling out an acute process and the peritoneal irritation, it was decided to perform an exploratory laparoscopy where hemoperitoneum was observed in four quadrants. Hemostasis was checked and a fluid sample was taken for cytology, which did not show atypical cells. A biopsy of the lesion was taken. The patient evolved with a requirement of 2 units of red blood cells after the procedure.
Electively, the computed tomography with intravenous contrast was repeated, revealing a polylobulated, heterogeneous, predominantly solid lesion, measuring 81x58x90 mm in the mesentery close to the right mesocolon, which displaces adjacent structures and enhances heterogeneously after the administration of contrast. Small mesenteric nodes are observed adjacent to the lesion, as well as heterogeneous free fluid in the pouch of Douglas (Figs. 1 and 2). Upper and lower digestive endoscopy and tumor markers were normal.
The pathological report showed retroperitoneal tumor of germinal origin. Negative flow cytometry for lymphoproliferative origin. The patient is discussed in an interdisciplinary committee, deciding resection. The procedure is performed laparotomically given the volume of the mass to be excised. A terminal ileum tumor associated with a large mass in the right mesocolon and peritoneal implants with a Sugarbaker scale of 5 were confirmed (Fig. 3). Right colectomy with the corresponding peritonectomy was performed to achieve an R0 radical resection (Fig. 4).
The final histopathology reports a GNET (Fig. 5) and translocation of the Ewing sarcoma breakpoint region 1 gene (EWSR1) using fluorescence in situ hybridization technique (FISH).
 |
Figure 1. CT scan. Axial section. Heterogeneous tumor with intravenous post-contrast enhancement.
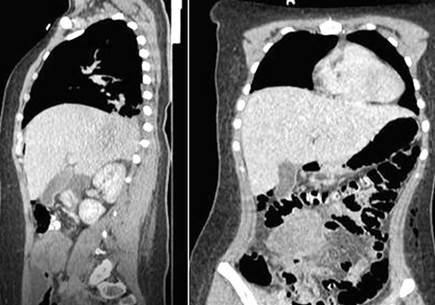
Figure 2. CT scan. Coronal and sagittal sections showing mass in the terminal ileum.
 |
 |
Figure 3. Tumor of the terminal ileum. Figure 4. Surgical specimen. Tumor of the terminal ileum with extension to the right mesocolon.
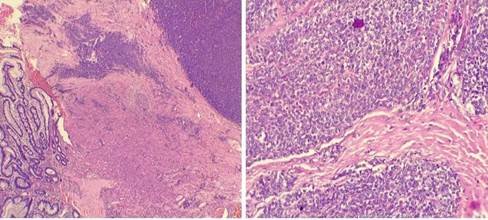 |
Figure 5. Histopathology showing epithelial cells grouped in nests and separated by fibrous septa, mainly in an extramucosal location.
The patient continues on oncologic treatment with cyclophosphamide + vincristine. Control CT revealed multiple heterogeneous nodular peritoneal images in the abdomen and pelvis with enhancement, surrounding the VI hepatic segment and the dome. Nodular images in the right intercostal wall and subcutaneous cellular tissue of the umbilical region. Free fluid in the abdominal cavity. Given the suspicion of bone marrow infiltration, a bone marrow aspirate was performed, which was positive. The patient evolves with symptoms of end stage intestinal cancer, including edema and ascites.
Although the majority of gastrointestinal mesenchymal tumors correspond to gastrointestinal stromal tumors (GIST), when expression of the KIT receptor is not found, other differential diagnoses should be considered, among which GNET stands out. In 2003, Zambrano et al3 reported 6 cases of primary tumors of the gastrointestinal tract with both histological and immunohistochemical differences with GIST, but similarities with clear cell sarcoma of soft tissues, classifying this tumor as a new entity. In 2012, Stockman et al4 were the first to present a series of 16 cases and call it GNET. The average age was 42 years, with no difference between sexes. The most common presentation was abdominal pain, intestinal obstruction, or discovery of a mass on imaging. The majority (62.5%) was found in the small intestine, most frequently in the ileum. 43% had liver metastases and 68% had lymph node metastases at the time of diagnosis. On the other hand, Chang et al5 reported 19 cases with 5.9% and 23% of liver and lymph node metastases, respectively.
Due to its heterogeneous histology,4 immunohistochemical study is essential for diagnosis. GNET has strong diffuse expression of the S-100 protein, which is unusual in GIST and rules out leiomyosarcoma. They are also characterized by the expression of SOX10 and the absence of melanocytic differentiation. Furthermore, they lack cytokeratin expression, which rules out carcinoma. When analyzing the genetic profile, GNETs present rearrangements of the EWSR1 gene on chromosome 22, detected using the FISH technique.3-5This pattern suggests
that these tumors originate from primitive cells related to the autonomic nervous system of the neural crest.1
Because it is an extremely rare disease, there is currently no standardized treatment. The vast majority included radical resection associated with lymphadenectomy, followed by strict follow-up to evaluate recurrence or metastasis. The adjuvant chemotherapy regimen is variable and includes alkylating agents, alkaloids or tyrosine kinase inhibitors.3,4
GNET is an extremely rare and difficult to diagnose tumor in which immunohistochemistry plays a fundamental role. The vast majority occur in middle-aged people, with the ileal location predominating. Although they may present with general symptoms such as asthenia, anemia, and weight loss, patients usually present with abdominal pain, intestinal obstruction, or a palpable abdominal mass.
There are few cases reported to date and there are no controlled studies on the treatment of this entity. The importance of new clinical studies is highlighted to standardize treatment and obtain better long-term results.
1. Friedrichs N, Testi MA, Moiraghi L, Modena P, Paggen E, Plötner A, et al. Clear cell sarcoma-like tumor with osteoclast-like giant cells in the small bowel: further evidence for a new tumor entity. Int J Surg Pathol. 2005;13:313-18.
2. González Ramírez DM, Velásquez JC, Quevedo Morales YA, Bonilla CE, Bruges RE. Tumor neuroectodérmico gastrointestinal maligno (GNET): a propósito de un caso. Rev Colomb Hematol Oncol. 2016; 3:38- 41.
3. Zambrano E, Reyes-Mugica M, Franchi A, Rosai J. An osteoclast-rich tumor of the gastrointestinal tract with features resembling clear cell sarcoma of soft parts: reports of 6 cases of a GIST simulator. Int J Surg Pathol. 2003; 11:75–81.
4. Stockman DL, Miettinen M, Suster S, Spagnolo D, Dominguez- Malagon H, Hornick JL, et al. Malignant gastrointestinal neuroectodermal tumor: clinicopathologic, immunohistochemical, ultrastructural, and molecular analysis of 16 cases with a reappraisal of clear cell sarcoma-like tumors of the gastrointestinal tract. Am J Surg Pathol. 2012; 36:857-68.
5. Chang B, Yu L, Guo WW, Sheng WQ, Wang L, Lao I, et al. Malignant gastrointestinal neuroectodermal tumor: clinicopathologic, immunohistochemical, and molecular analysis of 19 cases. Am J Surg Pathol. 2020; 44:456-66.