Laparoscopic left colectomy with intracorporeal anastomosis: initial experience
Davrieux Federico1,2, Marcucci Gustavo1, Lavallen Gustavo1, Giavaresco Ana1,
Lorenzi Lisandro1
1
Departamento de Cirugía, Sanatorio de la Mujer, Rosario, Santa Fe, Argentina.
2 Fundación DAICIM, Ciudad Autónoma de Buenos Aires, Buenos Aires, Argentina.
The authors declare no conflicts of interest
ABSTRACT
Background: Laparoscopic surgery has advanced in colorectal pathology. Reports of intracorporeal anastomosis in laparoscopic right colectomy are more common, as it appears to be less challenging. Intracorporeal anastomosis in left colectomy could maximize the benefits of laparoscopy while maintaining the same surgical safety.
Aim: To analyze the results of our initial experience in laparoscopic left colectomy with intracorporeal anastomosis.
Design: Retrospective, descriptive study.
Methods: Patients with a diagnosis of benign and malignant pathology of the left colon treated by surgery in a single center, between March 2021 and March 2022, were analyzed. The variables analyzed were demographics, surgical techniques, postoperative complications, operative time and hospital length of stay.
Results: A total of 18 patients (44.5% women, 55.5% men) with a mean age of 55 years were analyzed. Pathology was benign in 61.1% of patients and malignant in 38.9%. The type of anastomosis performed was side-to-side (72.2%), side-to-end (22.2%), and end-to-end (5.5%). Hand-sewn suture was performed in 72.2% of patients and stapled suture in 27.7%. The mean operative time was 126.5 minutes (p > 0.05). The mean hospital stay was 6 days (p>0.05). A complication rate of 33.3% and a relaparoscopy rate of 16.6% were reported. No conversions were recorded. There was no mortality.
Conclusions: Laparoscopic left colectomy with intracorporeal anastomosis is a safe technique. It allows you to take advantage of the benefits offered by laparoscopy. It requires an experienced surgical team with a high level of training in laparoscopic surgery and appropriate technology.
Key words: laparoscopic surgery, colorectal surgery, left colectomy, intracorporeal anastomosis
INTRODUCTION
Laparoscopic surgery has advanced remarkably in all fields. Its use in colorectal pathology has not been the exception, demonstrating comparable results with open procedures.1,2
Laparoscopic right colectomy appears to be less challenging than left colectomy. Perhaps for this reason, in right colectomy it is more frequent to observe reports of intracorporeal anastomosis, while in left colectomy extracorporeal anastomosis is more frequent.3 This variant is associated with a longer surgical wound and everything that this entails (greater postoperative pain, wound infections, operating time, cosmetic factor).4
Several authors consider that intracorporeal anastomosis in left colectomy could maximize the benefits of laparoscopy. Although the publications of this technique are isolated, to date it has been reported that it offers safety in terms of anastomosis and its complications (dehiscence, fistula, stenosis).5
The aim of this study was to analyze the results of our initial experience in laparoscopic left colectomy with intracorporeal anastomosis.
MATERIAL AND METHODS
This is a retrospective and descriptive study of patients diagnosed with benign and malignant disease of the left colon, treated by laparoscopic left colectomy with intracorporeal anastomosis. It was carried out at the Sanatorio de la Mujer in the city of Rosario, Santa Fe, Argentina, for 12 months, from March 2021 to March 2022. All patients were cared for by the same surgical team.
The following variables were analyzed: demographics (age, sex, pathology), operative technique (anastomosis preparation, type of suture used), postoperative complications (according to the Clavien-Dindo Classification),6 operative time (minutes) and length of stay (days).
The inclusion criteria were: 1) patient with benign pathology of the left colon (chronic fistula, acute and chronic left diverticular disease, traumatic lesion), 2) patient with left colon cancer.
The exclusion criteria were: severe coagulopathy, hemodynamic instability, peritoneal sepsis, signs or suspicion of associated intestinal ischemia, lack of patient cooperation.
The diagnosis was made through anamnesis, physical examination, blood tests, endoscopic studies and imaging studies such as Computed Tomography and Magnetic Resonance. The staging of the oncological disease and its possibility of surgical resection were performed.
In the preoperative period, all the patients underwent complete laboratory studies, identification of blood group and factor and the respective reserve of blood units, cardiological evaluation and electrocardiogram, chest X-ray and tetanus vaccination. In specific cases, complementary studies were carried out such as stress test, echocardiography, spirometry, among others.
Surgical technique
Surgery was performed under general anesthesia and with continuous monitoring of vital parameters by the anesthesiologist in charge. At the start of the procedure, a K-10 nasogastric tube and a 16 Fr Foley bladder catheter were placed. In the event of suspected ureteral involvement, a double J stent was implanted.
The laparoscopy equipment used was a high-definition video system (HD 1288®, Stryker, USA) programmed in “laparoscopy mode” accompanied by a light source (L9000®, Stryker, USA) with previous “balance of whites” and a carbon dioxide (CO2) insufflator (Pneumo Sure XL®, Striker, USA) that was programmed at high recovery flow (40 liters per minute) with a pressure of 12 mmHg.
An energy unit (Force Triad®, Medtronic, USA) with monopolar (hook type) and vessel-sealing forceps (LigaSure Blunt Tip®, Medtronic, USA) was used.
The patient was placed in supine position with legs open and Trendelenburg to favor mobilization of the omentum and small bowel loops. The main surgeon was positioned to the right of the patient, the first assistant to the left and the second assistant to the left of the surgeon (optical camera). The instrumentalist and the table were located to the right of the surgeon and the laparoscopy tower with its monitor in a caudal position in relation to the patient.
Veress needle pneumoperitoneum was established. Four trocars were used, arranged as follows: 10 mm umbilical trocar (optic and camera), 1 trocar in the right iliac fossa (12 mm for the stapling device), a 5-mm trocar in the right upper quadrant and a 5-mm trocar in the left iliac fossa (Fig. 1). An accessory trocar was sometimes used in the epigastrium to aid in mobilization of the colon and suturing.

Figure 1. Patient position and trocar placement for a laparoscopic left colectomy.
Surgery began with the exploration of the abdominal cavity to rule out extracolonic lesions not noticed in other studies (in case of malignant pathology). A lateral to medial dissection was performed. The first step was the dissection of the left Toldt's fascia with release of the splenic flexure. Dissection of the left mesocolon continued, with dissection of the inferior mesenteric vein up to the head of the pancreas for its preservation. Dissection of the mesocolon continued with special care of the ureter. Once the colon and part of the rectum had been mobilized, the vessels were identified and ligated with plastic clips (Hem-o-lock® System, Weck, Teleflex, USA). Once the colonic segment was freed and hemostasis controlled, it was sectioned with a linear stapler (Echelon Flex®, Ethicon-Johnson (Echelon Flex®, Ethicon-Johnson & Johnson, USA). The specimen was placed in a bag and extracted through a Pfannenstiel incision of less than 6 cm in length, protected with a wound protector (Alexis Wound Protector®, Applied Medical, USA) (Fig. 1). In other female patients the specimen was extracted through the vagina. The specimen was prepared and sent for pathology study. Subsequently, the intracorporeal colorectal anastomosis was performed, either hand-sewn or with curved or linear stapler (Fig. 2).
The specimen was prepared and sent for pathology study. Subsequently, the intracorporeal colorectal anastomosis was performed, either by hand or with a curved or linear stapler (Fig. 2). The tightness of the anastomosis was tested with the hydropneumatic test.
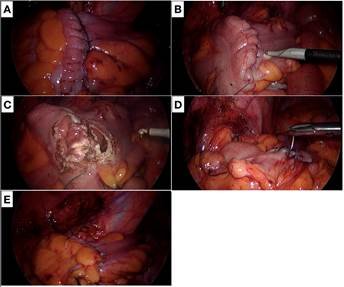
Figure 2. Laparoscopic left colectomy with intracorporeal anastomosis. A, B, and C. Preparation of the bowel ends and closure of the posterior border of the anastomosis. D and E. Closure of the antimesenteric border of the anastomosis with a double-layer hand-sewn suture.
A multifenestrated silicone drain was offered to the anastomosis and to the Douglas pouch and the abdominal wound was closed with a layered technique (Fig. 3).

Figure 3. Final cosmetic appearance, Pfannenstiel incision and drainage.
Postoperative follow-up
The patients remained in the intensive care unit during the immediate postoperative period. Gastric protection, antiemetics, analgesics, antibiotics, and deep vein thrombosis prophylaxis were administered in all cases. Transfer to the general ward and early enteral nutrition were then implemented. The removal of drains was gradual according to the quantitative and qualitative characteristics of the output.
Statistic analysis
Statistical data was analyzed using computer programs and expressed as mean, percentage, range, and standard deviation. For the statistical analysis of the variables, the Chi-square test was used. A value of p<0.05 was considered statistically significant.
Bioethical aspects
All patients were correctly informed and signed the consent for the surgical procedures and the use of their data in scientific publications.
RESULTS
Eighteen patients were analyzed, 44.5% women and 55.5% men, with a mean age of 55 years, 61.1% presented benign pathology and 38.9% malignant pathology (Table 1).
Table 1. Demographic variables.
|
N |
18 |
|
Age |
55 years (range 35-78) |
|
Sex |
8 women (44.5%) |
|
10 men (55.5%) |
|
|
Pathology |
|
|
Benign* |
11 (61.1%) |
|
Malignant† |
7 (38.9%) |
*Diverticular disease 7, fistulas 2 (recto-vaginal 1,
recto-vesical 1), high rectal tear 1, serrated polyp 1.
†Left colon cancer.
The anastomosis was side-to-side in 72.2% of the patients (n=13), side-to-end in 22.2% (n=4), and end-to-end in 5.5% (n=1). Manual suture was performed in 72.2% of the patients (n= 13) and stapled suture in 27.7% (n= 5) (Table 2).
The average operating time for the two techniques was 126.5 (range, 120-165) minutes, with no statistical significance between them (163 vs. 122 minutes for hand-sewn vs. stapled anastomosis, respectively).
|
Table 2. Surgical technique data. |
|||||||||||||
|
Pathology (n= 18) |
|
Anastomosis |
|||||||||||
|
|
Type |
||||||||||||
|
Side-Side |
Side-End |
End-End |
|||||||||||
|
Suture |
HS |
S: C |
S: L |
S |
S: C |
S: L |
S |
S: C |
S: L |
||||
|
Benign (n= 11) |
8 |
2 |
- |
- |
- |
- |
1 |
- |
- |
||||
|
Malignant (n= 7) |
|
|
- |
- |
3 |
4 |
- |
- |
- |
- |
- |
||
S: handsewn. S: stapled. C: curved stapler. LS: linear stapler.
The complication rate was 33.3% (n=6) (Table 3). Three of these 6 patients underwent reoperation, representing a relaparoscopy rate of 16.6%. No conversions to open surgery were recorded. There was no mortality.
The mean hospital stay was 6 (range, 3-10) days, with no statistical significance between the two techniques.
|
Table 3. Postoperative complications. |
||||||
|
N |
|
18 |
Clavien-Dindo Classification |
p |
||
|
Complications |
6 (33.3%) |
NS |
||||
|
Fistula* |
1 |
Grade IIIb |
||||
|
Contaminated hematoma* |
1 |
Grade IIIb |
||||
|
Acute abdomen* |
1 |
Grade IIIb |
||||
|
Febrile syndrome† |
1 |
Grade I |
||||
|
Postoperative ileus‡ |
1 |
Grade I |
||||
|
Urinary infection§ |
1 |
Grade I |
||||
|
Re-laparoscopies |
3 (16.6%) |
|||||
|
Conversions |
0 |
|||||
|
Mortality |
|
0 |
NS |
|||
|
NS: Not significant. *Required re-laparoscopy. †Good response to treatment after 7 days of hospital stay. ‡ Favorable outcome at 48 hours. §Good response to antibiotic treatment. |
||||||
DISCUSSION
The minimally invasive laparoscopic approach to the colon is well accepted by most of the surgical community, as it has been shown to reduce short-term morbidity and mortality.7,8
There are several reports on the technical feasibility and oncologic outcomes of laparoscopic right colectomy with intracorporeal anastomosis for colon cancer,9 as it is considered less challenging than left colectomy.5
Several studies comparing intracorporeal vs. extracorporeal anastomosis in laparoscopic right colectomy did not show statistically significant differences between the two groups.10-12 Therefore, different authors performed laparoscopic left colectomy with intracorporeal anastomosis, especially in colon cancer, obtaining good oncological results, maintaining the corresponding required safety standards.2 It was described as a technique with acceptable feasibility, a low complication rate, consistent cosmetic results, and reduced length of stay, which does not excessively prolong intraoperative time.13 However, many surgeons consider intracorporeal anastomosis to be technically difficult and could increase intraoperative time.
Milone et al.,5 in 2018 analyzed this discrepancy in a multi-institutional study on 181 patients who underwent intracorporeal vs. extracorporeal anastomosis after laparoscopic left colectomy for splenic flexure cancer. They reported good postoperative results with a low rate of complications and reoperations in the first group.
Even more controversial is the use of this technique in elective or emergency surgery for diverticular disease.14 However, the current trend is in that direction, as several studies and meta-analyses have shown good results, albeit without definitive conclusions.15,16
In the analysis of our series, it was observed that intracorporeal anastomosis in laparoscopic left colectomy was feasible and safe. There were no conversions and the rate of intra and postoperative complications was low. In addition to control of abdominal drainage, strict clinical control during the immediate postoperative period made it possible to detect complications early and act accordingly.
Beyond offering the benefits of laparoscopy, such as less abdominal injury and less postoperative pain, we believe that this technique allows the same anastomotic safety as other techniques and less traction on the mesocolon, with a lower rate of postoperative fistulas. Some authors maintain that this maneuver together with preservation of the inferior mesenteric vein could provide a better functional result and reduce anastomotic leakage.17
This study has some limitations, the main one being the small number of patients in the series. It would be advisable to carry out a large-volume, multicenter randomized clinical trial and compare patients undergoing laparoscopic left colectomy with intra vs. extracorporeal anastomosis. In this way it will be possible to determine the true impact of this technique.
Another limitation is the heterogeneous suture material used, both in hand-sewn (polyglactin vs. barbed) and stapled (linear vs. circular) anastomoses. Homogenization in this aspect could eliminate biases.
CONCLUSIONS
We found that laparoscopic left colectomy with intracorporeal anastomosis is a safe technique for the treatment of benign and malignant pathologies of the left colon. It allows taking advantage of the benefits offered by laparoscopy in terms of good tolerance to postoperative pain, less abdominal injury and rapid recovery of the patient.
However, we emphasize that an experienced surgical team is required, with a high level of training in laparoscopic surgery and adequate technology.
The correct selection of the patient and a strict postoperative clinical control are essential for the early diagnosis of complications related to the anastomosis.
REFERENCES
1. Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, et al. paroscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007; 142:298-303.
2. Wilson MZ, Hollenbeak CS, Stewart DB. Laparoscopic colectomy is associated with a lower incidence of postoperative complications than open colectomy: a propensity score-matched cohort analysis. Color Dis. 2014; 16:382-89.
3. van Oostendorp S, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J, et al. Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc. 2017; 31:64-77.
4. Campana JP, Pellegrini PA, Rossi GL, Ojea Quintana G, Mentz RE, Vaccaro CA. Right versus left laparoscopic colectomy for colon cancer: does side make any difference? Int J Colorectal Dis. 2017; 32:907-12.
5. Milone M, Angelini P, Berardi G, Burati M, Corcione F, Delrio P, et al. Intracorporeal versus extracorporeal anastomosis after laparoscopic left colectomy for splenic flexure cancer: results from a multi-institutional audit on 181 consecutive patients. Surg Endosc. 2018; 32:3467-73.
6. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205-13.
7. Lacy AM, García-Valdecasas JC, Piqué JM, Delgado S, Campo E, Bordas JM, et al. Short-term outcome analysis of a randomized study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc. 1995; 9:1101-5.
8. Arezzo A, Passera R, Ferri V, Gonella F, Cirocchi R, Morino M. Laparoscopic right colectomy reduces short-term mortality and morbidity. Results of a systematic review and meta-analysis. Int J Colorectal Dis. 2015; 30:1457-72.
9. Milone M, Elmore U, Di Salvo E, Delrio P, Bucci L, Ferulano GP, et al. Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc. 2015; 29:2314-20.
10. Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM, et al. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018; 24:2247-60.
11. Vignali A, Bissolati M, De Nardi P, Di Palo S, Staudacher C. Extracorporeal vs. Intracorporeal Ileocolic Stapled Anastomoses in Laparoscopic Right Colectomy: An Interim Analysis of a Randomized Clinical Trial. J Laparoendosc Adv Surg Tech A. 2016; 26:343-48.
12. Selvy M, Mattevi C, Slim K, Pezet D, Pereira B, Le Roy B. Intra-versus extracorporeal anastomosis in laparoscopic right colectomy: a meta-analysis of 3699 patients. Int J Colorectal Dis. 2020; 35:1673-80.
13. Swaid F, Sroka G, Madi H, Shteinberg D, Somri M, Matter I. Totally laparoscopic versus laparoscopic-assisted left colectomy for cancer: a retrospective review. Surg Endosc. 2016; 30:2481-88.
14. Di Saverio S, Vennix S, Birindelli A, Weber D, Lombardi R, Mandrioli M, et al. Pushing the envelope: laparoscopy and primary anastomosis are technically feasible in stable patients with Hinchey IV perforated acute diverticulitis and gross faeculent peritonitis. Surg Endosc. 2016; 30:5656-64.
15. Wu KL, Lee KC, Liu CC, Chen HH, Lu CC. Laparoscopic versus Open Surgery for Diverticulitis: A Systematic Review and Meta-Analysis. Dig Surg. 2017; 34:203-15.
16. Masoomi H, Buchberg B, Nguyen B, Tung V, Stamos MJ, Mills S. Outcomes of laparoscopic versus open colectomy in elective surgery for diverticulitis. World J Surg. 2011; 35:2143-48.
17. Melani AGF, Pandini RV, Lima MB, Bertulucci P, Spinelli A. Laparoscopic left colectomy with intracorporeal anastomosis: a complete mesocolic excision with preservation of the inferior mesenteric vein - a video vignette. Colorectal Dis. 2020; 22:2337.