Blunt anorectal
trauma. Case report and
literature review

Dayana
Naranjo Cardenas1, Ignacio Ramallo2, Rene Schumacher3,
Gisela Makarchuk1, Eliomar Aguilar1
General Surgery Service, Hospital Naval Puerto
Belgrano
1 Resident
2 Resident Instructor
3 Head of Service
|
|
ABSTRACT
Introduction:
Anorectal trauma is a rare cause of consultation to the Emergency Department,
with an incidence of 1 to 3%. It is often associated with life-threatening
injuries, so it is essential to know the principles of diagnosis and treatment,
as well as the initial care protocols for the polytraumatized patient.
Methods:
We present the case of a 47-year-old man with a blunt anorectal trauma
involving the internal and external anal sphincter, treated with primary
overlapping repair of the sphincter complex and suturing of the rectal wall. At 12 months the patient presents good outcome,
without anal incontinence.
Conclusion:
The treatment of rectal trauma, based on the 4 D´s dogma (debridement, fecal
diversion, presacral drainage, distal rectal washout) was successful. Repair of the overlapping sphincter injury was
simple and effective for anatomical and functional reconstruction.
Keywords: anorectal trauma, traumatic anal sphincter injury.
INTRODUCTION
Anorectal
trauma is a rare cause of emergency department consultation. The reported
incidence is 1 to 3% in civilian trauma centers and 5% in war scenarios.1,2
Its presentation is more common in men between 20 and 40 years old.
Anorectal injuries can be penetrating (56%), most frequently caused by knife
stab or gunshots, or blunt injuries (44%), due to traffic accidents (42%),
falls from a height (16%) and foreign bodies, among others (1%).3 They can
occur isolated or associated with injuries of other organs.
It is essential to know the principles of diagnosis
and treatment of anorectal injuries since they can be serious and, although
they do not increase mortality in the golden hour of trauma, they can increase
late mortality in the polytraumatized patient. For this reason, it is of utmost importance to provide
correct primary care based on the ABCDE of the Advance Trauma Life Support
(ATLS).
Once the patient is stabilized, secondary survey identifies anal or rectal
injuries that require early surgical intervention.1 Clinical
assessment should consider the etiology of trauma, interval since injury,
associated injuries, and symptoms, in addition to assessment of general
condition. Depending on the latter, the complementary method to be used will be
decided, with computed tomography being the most used due to its usefulness in
the polytraumatized patient.2
After the multi-institutional retrospective study published in 2018 by Brown,
et al.,1 the 4 Ds dogma (debridement, fecal diversion, presacral
drainage, distal washout) has become the treatment of choice for
extraperitoneal rectal injuries.
CASE
A 47-year-old male patient consulted the
emergency department due to rectal bleeding and subsequent perianal pain after
falling from 1.20 meters high onto a flat metal structure.
On physical examination, he was alert,
oriented, hemodynamically stable, lungs were clear, abdomen was soft,
nontender, nondistended, bowel sound present. BMI: 31.14 kg/ m2. He had a
hematoma and bleeding from a left anorectal tear with involvement of the sphincter
muscles and all layers of the rectum.
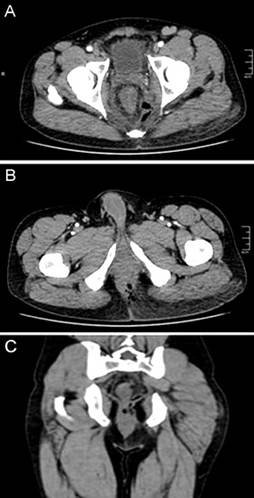
Given the hemodynamic stability, a
computed tomography scan was requested, which showed a tear in the left
internal
and external anal sphincter, associated
with air bubbles in the left mesorectum of the lower rectum (Fig. 1).
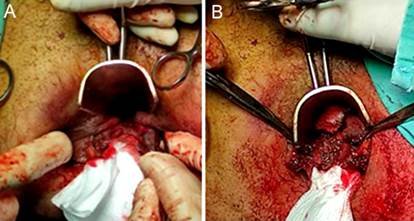
Once the surgical procedure was
decided, the patient was placed in the lithotomy position, after spinal
anesthesia. The injuries described previously were confirmed (Fig. 2A). A left
curvilinear incision from hour 7 to hour 3 was made and the devitalized tissue
of the presacral space, ischiorectal fossa, and left supralevator space were
debrided. After dissection of the internal and external anal sphincter,
suturing of all layers of the rectal wall and anal canal, with overlapping sphincter
repair were performed (Fig. 2B).
The skin was left open.
Drains were placed through counterincisions in the left
ischiorectal fossa and presacral space (Fig. 3). Loop sigmoid colostomy
was performed by laparotomy, with extensive distal washout.
On
the third postoperative day, a new surgical toilet of the wound was performed,
and the patient was discharged on the fifth postoperative day.
Anorectal manometry and dynamic magnetic resonance imaging (MRI) were performed
80 days postoperatively to evaluate sphincter function. Manometry showed
hypotensive internal anal sphincter, normotensive external anal sphincter,
inhibitory rectoanal reflex present, incomplete relaxation of the puborectalis
muscle during straining, and normal rectoanal sensation. Dynamic MRI revealed
alteration of the levator ani muscle and sphincters on the left side, in
relation to his surgical history, with adequate
contraction of the levator ani muscle.
Colostomy closure was performed 95 days after anorectal repair. The outcome was
good and the patient was discharged on the third postoperative day.
At the 12-month follow-up, the patient had good sphincter function without
incontinence, with a Wexner score of 0 (Fig. 4).
The authors declare no conflicts
of interest.Dayana Naranjo Cardenas: gayanaran@gmail.com
Received: July 2022. Accepted:
July 2023.
Dayana Naranjo: https://orcid.org/0000-0003-0544-4607, Ignacio Ramallo: https://orcid.org/0000-0001-5139-3586, Schumacher Rene: https://orcid.org/0000-0003-2619-1370,
Makarchuk Gisela: https://orcid.org/0000-0001-9776-0484, Aguilar Eliomar: https://orcid.org/0000-0001-6034-8664
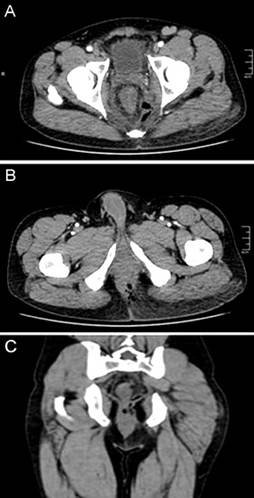
Figure 1. Pelvic CT
scan. Axial sections showing left anorectal injury.
A. Perirectal air
bubbles. B. Defect of the left sphincter complex with
perianal air bubbles. C. Coronal section with air bubbles in the
left
mesorectum of the inferior rectus.
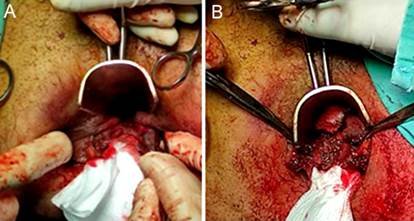
Figure 2. A. Tear of the posterior anal canal including the
sphincter complex. B. External anal sphincter repaired with
overlapping
technique.

Figure 3. Immediate
postoperative period. Open skin wound and
drains offered to the presacral space and left ischiorectal fossa.

Figure 4.
Late postoperative period.
DISCUSSION
Although traumatic anorectal injuries are rare, they
represent a challenge for the general surgeon due to their high morbidity and
mortality rate, which ranges between 3 and 10%, and their possible
postoperative complications of up to 21%.2
Anatomically, the anorectal region is protected by
the thighs, the pelvic bone girdle and the roots of the lower limbs,2
which makes diagnosis difficult and requires a high index of suspicion. For
detection, rectal examination, rigid
rectoscopy or sigmoidoscopy and triple contrast CT scan
of the abdomen and pelvis are essential, the latter being the standard method
as long as the patient is hemodynamically stable.
The treatment of anorectal trauma is based on the
principles of fecal diversion, distal washout, presacral drainage and
debridement (4 Ds) with the aim of preventing sepsis and preserving anal
sphincter function. This procedure should be carried out taking into account
the classification of rectal trauma proposed by the American Association for
the Surgery of Trauma (AAST) Table 1.3 Treatment recommendations are
classified into three groups depending on the location of the trauma:
intraperitoneal rectal, extraperitoneal rectal and/or anal. Intraperitoneal
injuries are treated the same as colonic injuries. If bowel diversion is
necessary, it should be performed close to the injury, preferably with a loop
colostomy with intraoperative maturation.1,3,5,6 If a pelvic
fracture is associated, the colostomy should be performed in the transverse
colon, close to the hepatic flexure.
In rectal trauma, it is recommended to debride the wound, repair the injury,
via a transanal route for the lower rectum and a transabdominal route for the
upper rectum, and create a diverting colostomy. In some cases, presacral
drainage and/or distal rectal washout may be necessary, maneuvers that should
not be included routinely, since they triple abdominal complications.4,6
In anal trauma with sphincter involvement, it is important to initially define
whether it is associated with an intraperitoneal or extraperitoneal rectal
injury and, accordingly, perform primary or deferred repair, with or without
colostomy.6 Depending on the location of the lesion (intra or
extraperitonal), a terminal or loop colostomy is recommended. It should be taken
into account that the end colostomy (Hartmann type) is a more complex
procedure, which is associated with greater morbidity both in its preparation
and in its reversal.2
Reconstruction of intestinal transit must be preceded by a colonoscopy, if it
has not been previously performed, and by studies to evaluate anorectal
function, including manometry, dynamic MRI, and/or endoanal ultrasound. There
is still no consensus on the waiting time to perform ostomy closure.
In our patient, after the anorectal function tests, the treatment was based on
the 4 pillars (4Ds)1,2,4 a sigmoid loop colostomy, hyperbaric
chamber sessions that improved the healing of the soft tissues and restauration
of bowel continuity at 95 days.
Table 1.
Rectum injury scale from the American Association for the Surgery of Trauma
(AAST).3
|
I
|
Contusion or hematoma without devascularization, or
partial-thickness laceration of the rectal wall
|
|
II
|
Fulll-thickness
laceration of the rectal wall <50% circumference
|
|
III
|
Fulll-thickness laceration of the rectal wall ≥50% circumference
|
|
IV
|
Desga Full-thickness
laceration with extension into the perineum
|
|
V
|
Devascularized rectal segment
|
CONCLUSION
Anorectal
trauma is rare and is often associated with serious injuries. The primary goal
of treatment is to control life-threatening lesions, minimize infection, and
preserve anal sphincter function. Among the multiple strategies described in
the literature, in our case we opted for the treatment based on the 4 pillars
and the reconstruction of sphincters with the overlapping technique, obtaining
good results.
REFERENCES
1. Torres Alcalá JT. Traumatismos
anorrectales. Protocolo de actuación. Cir Andal. 2018; 29:462-66.
2. McKnight GHO, Yalamanchili S, Sanchez-Thompson N,
Guidozzi N, Dunhill-Turner N, Holborow A,4 et al. Penetrating
gluteal injuries in North West London: a retrospective
cohort study and initial management guideline. Trauma Surg Acute
Care Open. 2021; 6:e000727.
3. Assenza M, Ciccarone F, Santillo S,
Mazzarella G, De Meis E, Bracchetti G, et al. Perineal trauma with anal
avulsion:
case report. Clin Ter. 2020; 170:e1-e6.
4. Ahern DP, Kelly ME, Courtney D, Rausa E,
Winter DC. The management of penetrating
rectal and anal trauma: a sys-
tematic review. Injury. 2017; 48:1133-38.
5. Scott SM,
Carrington EV. The London Classification: improving characterization and
classification of anorectal function
with anorectal manometry. Curr Gastroenterol Rep. 2020;
22: 55.
6. Lawrence Lee
MD. Management of trauma to the rectum and anus. Dis Colon Rectum. 2018;
61:1245-49.
![]()