Massive gastrointestinal bleeding as a presentation of a Meckel's diverticulum
Sergio Schlain1, Rocío Pérez Domínguez2, Hernán Alejandro Santilli2
1: Coordinador de Coloproctología, Instituto Médico Clínica de La Ribera. Ensenada, Provincia de Buenos Aires. 2: Staff de Coloproctología, Instituto Médico Clínica de La Ribera. Ensenada, Provincia de Buenos Aires
The authors declare no conflicts of interest.
Sergio Schlain: sergioschlain@hotmail.com
Received: March 2022. Accepted: October 2022
Schlain Sergio: 0002-5615-3503
Rocio Perez Dominguez: 0001-8347-0849
Hernan Alejandro Santilli: 0001-6749-0655
ABSTRACT
Meckel's diverticulum, the most common congenital malformation of the gastrointestinal tract, represents incomplete involution of the omphalomesenteric duct. Its bleeding is relatively common in children but not in adults, so its identification as a cause of this complication becomes more difficult. We present a rare case of severe lower gastrointestinal bleeding in a 17-year-old male due to a Meckel's diverticulum with heterotopic gastric mucosa. In the absence of precise imaging findings, although with high clinical presumption, laparoscopy made it possible to reach the diagnosis, identify the diverticulum and perform its resection, all in a single operative act.
Keywords: Diverticulum; Meckel; Hemorrhage; Complications
INTRODUCTION
Meckel's diverticulum, with an incidence of 2-4%, is the most frequent congenital malformation of the digestive tract.1It represents the incomplete involution of the omphalomesenteric duct normally obliterated in the fifth week of intrauterine life2 and is located at a mean distance of 46 cm from the ileocecal valve.
The form of presentation is diverse, depending on the age. It may only be an intraoperative finding during abdominal surgery for another cause, or it may present with a complication in the form of gastrointestinal bleeding, intestinal obstruction, or diverticulitis or meckelitis.
The cause of intradiverticular bleeding can be explained from the etiopathogenesis. There is presence of heterotopic mucosa inside the diverticulum, mainly gastric and less frequently pancreatic. Therefore, repeated secretion from these ectopic tissues leads to ulceration of the surrounding ileal mucosa, with consequent bleeding. It can occur acutely, in the form of rapid and massive bleeding, or insidiously with melenic feces.
Bleeding is a relatively frequent complication in children, in adults it is the second in order of frequency after obstruction, so it is not usually considered within lower gastrointestinal bleeding.
For diagnosis, imaging studies usually have low sensitivity and specificity.
Surgical treatment with resection of the diverticulum is mandatory in the presence of complications.
We present a rare case in an adult patient of gastrointestinal bleeding originating from a Meckel's diverticulum that required emergency surgery.
CASE
A 17-year-old male patient, with no pathological history, consulted due to 3-day history of melenic bowel movements, accentuated in the last hours.
Physical examination: patient with fair general condition, pallor, tachycardia, and slightly distended, soft, non-tender abdomen, without guarding. Proctologic examination: normal sphincter tone, scant traces of soft stool in rectal ampulla, gloved finger with blood.
He was admitted with a diagnosis of gastrointestinal bleeding, with hematocrit: 19% and hemoglobin: 6.2 g/dl. Treatment was started according to the protocol, with 2000 ml of lactated Ringer's solution and two units of packed red blood cells, obtaining a favorable response.
Upper digestive endoscopy: no lesions or bleeding sites were found. Subsequently, the patient presented an episode of syncope secondary to acute rebleeding with BP 80/50, HR 125 bpm and SatO2 98% with a mask, signs that appear after orthostatism. Transfer to intensive care is decided.
Abdominal and pelvic tomography with oral and intravenous contrast: a tubular image with a blind cul-de-sac with contrast inside is observed in the pelvis, which may correspond to an intestinal diverticulum (Fig. 1).

Figure 1. Abdominal computed tomography showing a tubular image in the pelvis with a blind cul-de-sac and contrast inside.
Angiography revealed no evidence of active bleeding.
Colonoscopy: blood remains in the entire colon and the last 20 cm of the ileum, without identification of the active site of bleeding.
Given the presumed diagnosis of bleeding from the small intestine due to a complicated Meckel's diverticulum, exploratory laparoscopy was performed. This shows a marked dilation of the colon and small intestine with suspicion of blood content inside and the presence of a diverticular sac 50 cm from the ileocecal valve, with a 4 cm neck and an approximate length of 10 cm, adhered to the greater omentum. Diverticulectomy and closure with stapling is performed, with subsequent reinforcement of the suture line with polyglactin 000 (Fig. 2). A multifenestrated drain is placed in the pouch of Douglas.
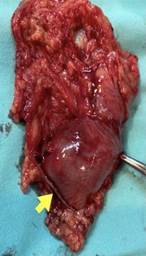
Figure 2. Resected specimen with the stapled suture line at the base of the diverticulum (arrow).
The patient was transferred to the Critical Care Unit, where he was extubated after resuscitation. On the first postoperative day he was hemodynamically stable, with a hematocrit of 29% and hemoglobin of 9.8 g/dl, for which he was transferred to the ward. On the second postoperative day, tolerating the diet he was discharged from hospital.
Histopathology examination: polypoid projections of the diverticular mucosa, made up of gastric epithelium with fundic glands and ectopic pancreatic tissue (Fig. 3).
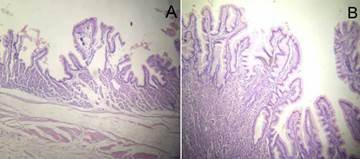
Figure 3. Histopathology of Meckel's diverticulum. A. Wall of the small intestine with polypoid projections from the mucosa, consisting of gastric epithelium and fundic glands. B. Heterotopic mucosa.
DISCUSSION
The diagnosis of Meckel's diverticulum complications is challenging due to the variability in its form and age of presentation.
According to the study published by Hansen and Søreide,3 46.7% of children with symptomatic Meckel´s diverticulum present obstruction, 25.3% gastrointestinal bleeding, and 19.5% inflammation. Obstruction, due to intussusception or fibrous band extending from the diverticulum to the umbilicus, is also the most common complication in adults (14-53%), followed by ulceration (<4%), acute or chronic diverticulitis and perforation. Whatever the cause of the obstruction, the presentation is similar: constipation, crampy abdominal pain, bilious vomiting, and abdominal distension.
In adults, about 80% of gastrointestinal bleeding is high and originates proximal to the ligament of Treitz; the rest are lower gastrointestinal bleeding whose most common source is the colon and in less than 5% the small intestine.
The usual studies include endoscopy of the upper and lower gastrointestinal tract, as well as the usual biochemical and hematological tests. In lower gastrointestinal bleeding, colonoscopy should be considered as the initial study, although in 25-32% of cases the origin of the bleeding is not found.4
CT angiography, when the bleeding rate is greater than 0.3-1.0 ml/min, has a sensitivity of 79-95% and a specificity of 95-100%. It should be considered first-line in active intestinal bleeding,5 since it can be performed in unstable patients and locate the source of bleeding in both the colon and the small intestine without the need for intestinal preparation.
Angiography detects extravasations of intraluminal contrast with bleeding of 0.5 ml/min or more and sometimes determines the cause. It has a sensitivity of 58-86% in lower gastrointestinal bleeding.4
Nuclear scan with Tc-99m pertechnetate can visualize Meckel's diverticulum, demonstrating simultaneous focal uptake of the radiotracer in normal and heterotopic gastric tissue. In children, it has a sensitivity of 80-90%, a specificity of 95%, and an accuracy of 90%, but in adults it is less reliable with a sensitivity of 62.5%, a specificity of 9%, and an accuracy of 46%.1 False negatives occur in those diverticula that do not contain ectopic gastric mucosa or when the number of gastric cells is inadequate for the concentration of the radiotracer.6
Preoperative diagnosis remains a challenge,7 less than 10% of symptomatic cases are diagnosed before surgery.8 Although there are a variety of diagnostic methods, they are not available in all institutions and even when they are, in some cases the etiology of the bleeding remains unclear.
Open surgery was for a long time the only effective method for the resolution of complicated Meckel's diverticulum. However, in the era of minimally invasive surgery, the laparoscopic approach represents a safe, cost-effective, and efficient method for diagnosis and treatment.9-11
Surgical resection is the treatment of choice and can be achieved by diverticulectomy or segmental bowel resection with primary anastomosis.5,3,12 Intestinal stapling devices (for open or laparoscopic surgery) have become useful tools due to their proven safety and ease of use.9,13
CONCLUSION
A rare case of massive lower gastrointestinal bleeding in the adult originating in the small intestine, in a Meckel's diverticulum, was presented. Given the lack of accurate imaging findings but with a high clinical presumption, laparoscopy allowed the diagnosis of the diverticulum and its resection in the same surgical procedure.
REFERENCES
1. Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med. 2006; 99:501-5.
2. Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Divertículo de Meckel: la experiencia de Mayo Clinic con 1476 pacientes (1950-2002). Ann Surg. 2005; 241:529-33.
3. Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore). 2018; 97:e12154.
4. Quiroga Gómez M, Pérez Lafuente M, Abu-Suboh A, Castell Conesa J. Hemorragia digestiva: papel de la radiología. Radiología. 2011; 53:406-20.
5. Oakland K, Chadwick G, East JE, Guy R, Humphries A, Jairath V, et al. Diagnosis and management of acute lower gastrointestinal bleeding: guidelines from the British Society of Gastroenterology. Gut. 2019; 68:776-89.
6. Levy A. Meckel diverticulum: radiologic features with pathologic correlation. RadioGraphics. 2004; 24:565-87.
7. Pedro F, Romano J, Rebelo M, Matias R, Carmo E. Catastrophic gastrointestinal bleeding: always consider Meckel's diverticulum. Eur J Case Rep Intern Med. 2019; 6:001224.
8. Willet A, Cortez N, Lobaton Y, Giubilei F, Nunez Herrero L. Obscure gastrointestinal bleeding from a Meckel’s diverticulum in a young adult: a challenging diagnosis. Am J Gastroenterol. 2021; 116: S1262.
9. Martin JP, Connor PD, Charles K. Meckel's diverticulum. Am Fam Physician. 2000; 61:1037-42.
10. Sanders LE. Laparoscopic treatment of Meckel's diverticulum. Surg Endosc. 1995; 9: 724-27.
11. Chan KW, Lee KH, Mou JWC, Cheung ST, Tam YH. Laparoscopic management of complicated Meckel’s diverticulum in children: a 10-year review. Surg Endosc. 2008; 22:1509-12.
12. Irie T, Shinji S, Arai H, Kan H, Yamada T, Koizumi M, et al. Intestinal hemorrhage caused by Meckel’s diverticulum with ectopic gastric mucosa on polypoid lesion: a case report. Surg Case Rep. 2016; 2:124.
13. DiGiacomo J. Cottone F. Surgical treatment of Meckelʼs diverticulum. South
Med J. 1993; 86:671-75.
COMMENT
Being in front of a patient with gastrointestinal bleeding and unkwon source after the endoscopic studies always implies a challenge for the treating medical team. Many times you have to deal with the pressure of those who believe exploratory surgery is convenient even without having exhausted the available diagnostic studies. Even more so when the clinical state of the patient requires rapid decision-making.
This situation was very well resolved in the case presented. They performed an adequate resuscitation that gave them the time and the opportunity to carry out the necessary studies to reach the diagnosis. The CT was the one that best oriented towards a Meckel's diverticulum.
You can have all the tools available, but you have to know how to manage them, as this case exemplifies.
With the diagnosis, I believe that the laparoscopic approach and resection of the diverticulum by this route was the best decision.
Sebastián Guckenheimer
Hospital
Dr. I. Pirovano, Ciudad de Buenos Aires, Argentina.